News
May 4, 2016
By Nuritas
No More Needles! Tattoos, Contact Lenses and Infrared Lights to Measure Blood Glucose

By Niamh Maire Mohan
Glucose fuels our bodies and our brains. Research has shown that having low glucose levels or “hypoglycaemia” can compromise the ability to make important decisions, impair self-control and willpower and dampen enthusiasm (Fairclough & Houston, 2004; Gailliot et al., 2007). Excessive glucose or “hyperglycaemia” in the bloodstream can have even greater consequences for health. Insulin is a hormone which regulates the metabolism of carbohydrates by encouraging the absorption of glucose to muscles as energy and to fat stores. Diabetes type 1 occurs when insufficient insulin is produced to deal with the sugar circulating in the blood whereas type 2 arises when the insulin produced is not used properly. The number of people with type 2 diabetes has quadrupled in the last 35 years and is interlinked in the web of risk factors for obesity, cancer, stroke and cardiovascular disease (World Health Organisation, 2016). Type 1 diabetes is controlled with multiple daily insulin injections whereas type 2 involves implementing a healthier lifestyle in combination with medication and, in some cases, injectable insulin.
The regular painful monitoring of blood glucose is a burden on patients, public health and the environment as the requirement to produce and dispose of used needles is dramatically increasing. Top research facilities around the world are searching for alternative pain-free, environmentally friendly methods to replace the ritual of finger pricking. Here are a few interesting examples:
Google Contact Lens – This clever technology uses a sensor in a wireless chip which is embedded in a contact lens to measure glucose levels in tears (Otis & Parviz, 2014). This technology, although still in the prototype stages, would allow for a glucose reading each second, thus providing a more continuous approach than finger pricking. Apps are being developed which could give patients and doctors access to the recorded measurements.
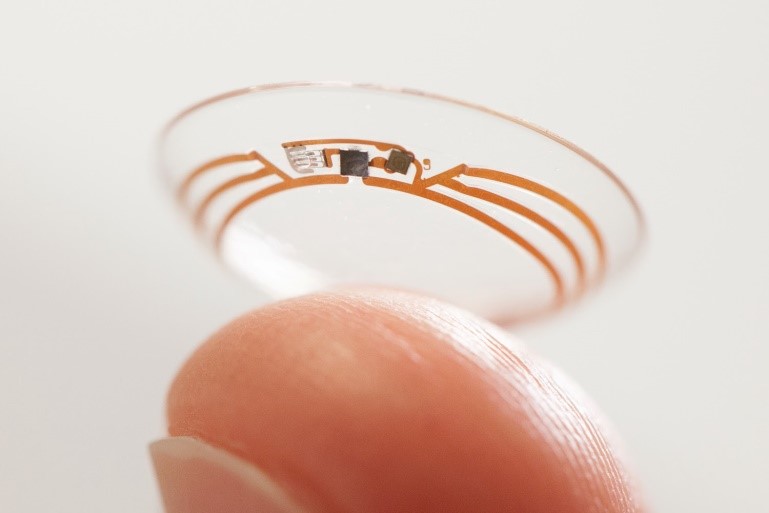
Photo source: Forbes.com
Diabetes Tattoos – “Nano-Tattoos” are invisible to the human eye but biologically active as the nanoparticles injected into the dermis act as continuous sensors to blood glucose (Barannikov, 2012). When exposed to UV light, the biomarkers emit light the intensity of which is proportional to the concentration of blood sugar. An app is being designed which can convert the intensity of the light into a glucose reading. The tattoo could also be designed to measure electrolyte imbalance in runners. A similar idea using a temporary tattoo has been designed in California where a stick on patch containing woven electrodes measures glucose from the sodium and glucose ion between skin cells when a mild current is applied (Mc Donald, 2015). Similar to the above technologies, the development of a user friendly way of interpreting the readout is underway.

Photo source: Popsci.com/Jacobs School of Engineering/UC San Diego
Infrared Lights – The technology was developed by researchers in Tohoku University in Japan. They advanced on the idea that glucose absorbs light at a specific wavelength; therefore when a pulse of infrared light is applied to thin skin, such as the inside of the mouth, it is possible to measure the levels present in the blood while barely penetrating the skin (Matsuura, 2016). The application of infrared light technology to replace blood strip tests is still being investigated, as the sensitivity of the technique needs improving, but is expected to be employed as an alternative method in the coming years.
Various other products already exist on the market such as Glucotrack which simultaneously uses ultrasonic, electromagnetic and thermal technologies to measure blood glucose or Glucowise which measures glucose at the capillary level by transmitting a low power radio wave through the thumb or earlobe.
Here at Nuritas, we love exciting new technology and the area of type 2 diabetes as well as pre-diabetes is of great interest to us. We are working hard on creating ingredients that will help in the prevention of many such chronic diseases.
References:
Barannikov, K., 2012. Nano-based treatment for diabetics is set to shine. The Guardian.
Fairclough, S. & Houston, K., 2004. A metabolic measure of mental effort. Biological Psychology, 66(2), 177–190.
Gailliot, M., Baumeister, R., DeWall, C., Plant, A., Brewer, L., Schmeichel, B., Tice, D. & Maner, J., 2007. Self-Control Relies on Glucose as a Limited Energy Source: Willpower is More than a Metaphor. Personal Soc. Psychology, 9(2), 352–336.
Huang, S. & Czech, M., 2007. The GLUT4 Glucose Transporter. Cell Metabolism, 5(4), 237–252.
Matsuura, Y., 2016. Invasive measurement of Blood Glucose No longer Necessary. Research News.
Mc Donald, F., 2015. This temporary tattoo can monitor diabetics’ glucose levels as accurately as a finger prick. [Online] Available at: http://www.sciencealert.com/scientists-have-made-a-temporary-tattoo-that-monitors-diabetics-glucose-levels-and-it-looks-awesome?action_object_map[635276886598791]= [Accessed 15/04/16].
Otis, B. & Parviz, B., 2014. Introducing out smart contact lens project. [Online] Available at: https://googleblog.blogspot.ie/2014/01/introducing-our-smart-contact-lens.html [Accessed 15/04/16].
World Health Organisation, W., 2016. Diabetes Factsheet. [Online] Available at: http://www.who.int/mediacentre/factsheets/fs312/en/ [Accessed 15/04/16].





 Previous
Previous
